
Health systems across the country will require a plan to react to government deep spending cuts and revenue shortfalls due to the COVID-19 pandemic. Hospital services have seen a significant downturn in demand in 2020, and the recent resurgence in cases has led to further decreases. The public health emergency has also resulted in innovation, most notably telehealth, which has been granted temporary pay parity during the pandemic.
Still, hospitals and health systems face a year of losses, but COVID-19 consequences like enhanced communication and flexible decision-making make now the time to adopt a cost-reduction care delivery model. I propose a widespread overhaul of all aspects of the care model to achieve system-wide cost-reduction. This should include using data analytics and feedback to evaluate service lines, the transition to low-cost care methods, and realign partners and payers towards a cost-reduction model.
Success will be measured by cost savings and patient satisfaction in permanently changing patient expectations, especially as payers continue the shift towards value-based reimbursement. This highly customizable model I propose can be tailored to any health system.
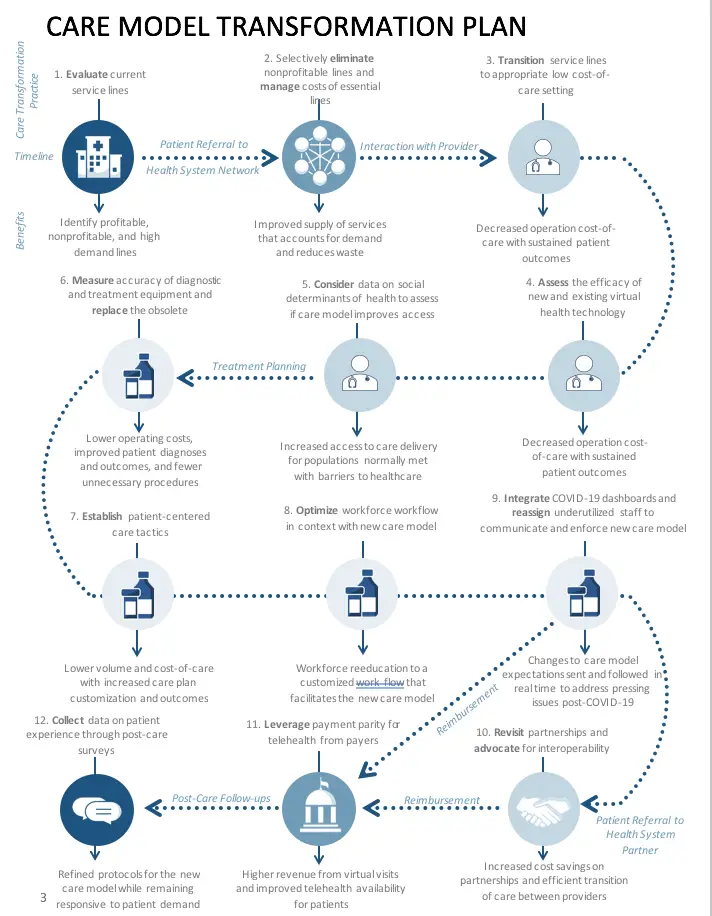
1. Evaluate current service lines.
Transforming each service line to a lower cost-of-care setting may not be possible. Those lines that are not bringing in stable revenue and are resistant to low-cost settings represent a drain on resources at a time where minimizing losses is paramount. Health systems should evaluate their existing services portfolio using data analytics, considering revenue, patient satisfaction, outcomes, operating costs, and potential for transformation to a lower cost-of-care setting.
2. Eliminate nonprofitable lines and manage costs of essential lines.
Because health systems today tend to be highly consolidated, there may be a wide range of profitable, nonprofitable, and essential lines. Nonprofitable lines that do not support quality patient outcomes and incur high operating costs or low reimbursement rates should be eliminated from the service mix. Reevaluating essential services can also reveal ways to manage high costs. This step results in a more focused and efficient heath system with reduced waste and an improved service portfolio.
3. Transition service lines to appropriate low-cost-of-care settings.
Each service line must be fit to an appropriate low-cost care model, like telehealth. The public health emergency made transitioning to virtual healthcare a necessity with the cost and patient satisfaction benefits it presents. Again, the use of big data and data informatics are essential in identifying where transitioning to virtual platforms is advantageous. Other strategies can be used in conjunction with telehealth, like preventative health service lines to reduce ER overutilization and rehospitalizations. Not all service lines will be conducive to a virtual setting. Alternate cost-effective and successful care settings include home healthcare, mobile healthcare units, home monitoring, and out-of-network partnerships.
4. Assess the efficacy of new and existing virtual health technology.
Existing virtual capabilities developed during the pandemic must be evaluated in a post-COVID-19 setting. Not all processes should be kept in this transition, and ineffective technologies could represent a further drain on hospital revenue without producing favorable results.
5. Measure accuracy of diagnostic and treatment equipment and replace the obsolete.
Obsolete technology represents money trapped in assets, especially real estate. Although investing in new technology raises costs in the short-term, the cost-reduction benefits that arise from lower operating costs, more efficient and accurate testing and diagnosis, and less unnecessary testing will more than makeup for the initial investment. Health systems should consider the investment of money and time in relation to the benefits when deciding which service lines should receive updated equipment. Again, data analytics can assess current asset performance and present opportunities for renovation.
6. Establish patient-centered care tactics.
Patient-centered care aligns with value-based care trends arising in payer reimbursement plans. This approach to care delivery reduces waste and unnecessary treatments, decreasing healthcare costs1 and improving patient outcomes and engagement2,3. Orienting the workforce towards delivering patient-centered care is a matter of culture change. Providers are encouraged to cut down on treatment volume and focus on treatment quality, saving the patient and the provider time and money.
7. Optimize provider workflow in context with the new care model.
The workforce will also require reeducation to operate new workflows associated with the cost-reduction model. Office setups, electronic health records, billing, and other aspects of workflow logistics will have to be rewritten. Modifications will require coordination from provider feedback, health IT, administrative staff, and reimbursement to be instituted efficiently into the everyday workflow.
8. Integrate COVID-19 dashboards and reassign underutilized staff to communicate and enforce the new care model.
Health systems have opened communication lines that directly connect management and decision-making boards to all members of the workforce. The urgency in relaying decisions was paramount during the health crisis, and it will remain crucial to facilitate the execution of any changes to workflow and treatment protocols that accompany the new care model. Reassigning underutilized staff to enforce new policies can help monitor the care model’s progression.
9. Revisit partnerships and advocate for interoperability.
Health systems must shift to a “coopetition” model and operate through strategically aligned partners. Health systems should revisit partnerships with external agencies to determine if there are any opportunities to negotiate or modify the agreement to match the new care model and mutually benefit both parties. Where no advantageous partnerships exist, expand in-network capabilities. Partnerships are also a tool to expand coverage in areas that are in high demand post-pandemic, including home care and mental and behavioral health. Interoperability application programming interfaces (APIs) ensure there is effective and safe coordination of care between partners and in-network providers, which will significantly decrease administrative stress and facilitate secure transitions of care in addition to added capabilities with remote monitoring devices on the rise.
10. Leverage payment parity for telehealth from payers.
Many fear that telehealth payment parity policies will not be upheld after the pandemic. Records of cost-reduction, higher patient outcomes, and stimulated patient and workforce engagement should be kept as evidence to leverage better telemedicine service coverage from payers. Health systems should freely share their successful results with payers and other health systems to encourage industry-wide virtualization and telehealth reimbursement. In fact, consortiums such as the Alliance for Connected Care exist with a public call for data to support concerted efforts.
11. Constantly reevaluate and improve.
More than ever, patients are showing drastic changes in their care delivery expectations, and health systems must be open to receiving feedback from consumers. Paying special attention to the needs of underrepresented patient populations that traditionally lack access will allow a more inclusive patient care model. Cooperation between health IT, technology developers, third-party telehealth vendors, and the workforce is essential in building customized virtual platforms. Cycles of trials including analytics and feedback will produce successful iterations to produce a final, optimized workflow.
About Moha Desai
Moha Desai is a Principal of Healthcare Strategy and Transformation where she focuses on driving forward strategic, planning, financial, revenue cycle, operational improvement, and patient engagement healthcare projects for providers, federal government health agencies, and various firms requiring growth, business development, and project implementation and management. She has previously served in leadership roles at Partners HealthCare, Deloitte Consulting, Bearing Point, etc. Moha received her B.A. in Economics from Columbia University and her M.B.A. at Yale University.
References:
1. Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229-239. doi:10.3122/jabfm.2011.03.100170
2. Priorities in Focus – Person- and Family-Centered Care | Agency for Health Research and Quality. Accessed August 26, 2020. https://www.ahrq.gov/workingforquality/reports/priorities-in-focus/priorities-in-focus-person-family-centeredcare.html
3. Kuehn BM. Patient-Centered Care Model Demands Better Physician-Patient Communication. JAMA. 2012;307(5):441-442. doi:10.1001/jama.2012.46