The material cost of COVID-19 has been at the center of public discourse since the early days of the pandemic. In 2020, growth in federal government spending on healthcare increased 36 percent, compared to the 5.9 percent bump in 2019. While the distribution of vaccines has allowed for a version of pre-pandemic life to resume, hospitals are still not recovered from the high rates of hospitalizations that occurred in March 2020, and the indirect costs of the pandemic continue to loom over the American population as a result of strained health systems.
During the early days, the cost of hospitalizing a patient seemed obvious: the sheer volume of long stays, expensive ventilators, a lack of one-size-fits-all treatment solutions, and the pause of elective surgeries. Now, Covid-19 continues to wreak havoc on our health systems, but in a more covert way. With only 4% of Americans fully boosted as we move into this winter’s ‘triple-demic’ – and long covid impacting the lives of as many as 16 million people on a daily basis – it’s clear that public health officials need to do more in order to support the American population and our struggling health systems.
The Cost of Healthcare Provider Burnout
Across the country, healthcare providers are reporting extreme rates of burnout. It is important to underscore that healthcare providers and hospital systems were stressed prior to Covid-19, but the pandemic has exacerbated it. Employment across healthcare is down 1.3 percent, or 223,000 jobs, from pre-pandemic levels. Over 90 percent of nurses said they are considering quitting their jobs by the end of 2022 in a survey, with 72 percent of nurses stating they had already experienced burnout before March 2020. In addition, the increased stress that doctors have experienced is resulting in worse patient care – with 28% of doctors who reported burnout sharing that the quality of care they are providing has significantly declined.
We are amid a mass healthcare provider exodus, and, according to estimates, each instance of physician turnover costs healthcare organizations at least $500,000, and each instance of staff registered nurse (RN) turnover costs $46,100. Without proper staffing, hospitals are at risk of closure and patients’ health is at risk of worsening.
The Cost of Hospital Closures
Before the pandemic, hospitals closed for several reasons, including insufficient staffing, lack of funding, and/or having a large uninsured patient population. Since March 2020, 21 hospitals across the United States, predominantly in rural areas, have closed. Health systems are still recovering from the significant loss of revenue from canceled appointments – according to a report from The Chartis Center for Rural Health, 82 percent of the rural hospitals surveyed said suspension of outpatient services resulted in a loss of at least $5 million per month.
So, what happens when hospitals and health systems close?
Rural areas experience more Covid-19-related deaths than urban communities and public health experts attribute these deaths to the rampant hospital closures, as well as a general lack of healthcare providers. It is a vicious cycle: Covid-19 strains hospital systems, healthcare professionals leave, hospitals close, and more patients will die from infectious diseases like Covid-19, the flu or respiratory syncytial virus (RSV) – not to mention the other reverberating public health complications that come as a result of these closures. Vaccinations have helped these hospitals stabilize, but to keep up with covid fatigue and the ever-evolving variants we need a variety of treatments in our arsenal.
More Covid-19 Treatments Will Bolster Struggling Health Systems
Increasing the number of vaccinated individuals around the world, in addition to broadening access to effective non-vaccine treatments, such as antivirals and monoclonal antibody therapies, will significantly lessen the impact of the disease on individuals and lessen the burden on the healthcare system. Antiviral treatments have proven to reduce hospitalization, but diversity in treatments is essential to keep up with the ever-evolving Covid-19 variants. Dr. Andrew Pavia, chief of pediatric infectious diseases at the University of Utah Health, was quoted on the effectiveness of antivirals: “If there is anything we know about viruses and antiviral drugs is that eventually, we will see some sort of resistance.” For the time being, antivirals are effective – this is not a call to leverage one type of therapy over another – this is a call to help patients and our health systems survive by equipping healthcare professionals with as many treatments as possible.
One such treatment that has proven highly effective when applied properly are neutralizing monoclonal antibody therapies. Like antivirals, monoclonal antibodies reduce hospitalization, the risk of death, and shorten the length of the infection – resulting in better patient outcomes and stronger health systems.
According to Yale Medicine, it is estimated that about three percent of the United States population, or up to 25 million individuals, is considered moderately-to-severely immunocompromised, making them more at risk for serious illness if they contract Covid-19, or other viruses. Monoclonal antibodies are a highly safe and efficacious treatment, which is extremely important for this vulnerable population, especially as a complement to vaccines for prevention. An infusion can reduce the risk of hospitalization by 80 percent or more in a high-risk person, and unlike antivirals, monoclonal antibodies target specific parts of the virus spike protein leading to fewer side effects and interactions with other drugs.
Collaboration between the government and the biotech industry will be essential for creating a portfolio of therapies to treat a variety of patient profiles who experience a range of Covid-19-related health issues. With our healthcare systems in such a precarious state, investing resources in the development of these treatments will prepare hospitals for future variants that threaten the health of our nation. The hope is that by bulking up our Covid-19 hospital response strategy, our already volatile health system will have a chance to recover, increase individuals’ access to quality healthcare, and ensure a healthier population.
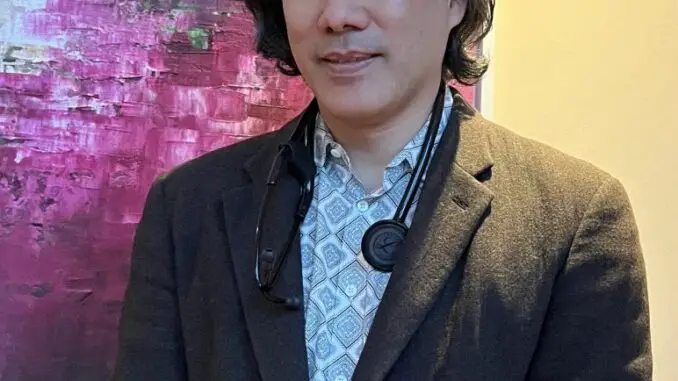
About Eugene Y. Chan, MD
Dr. Chan is a physician-inventor. He is currently Chairman, Co-Founder of Abpro, CEO of rHEALTH, and President, CSO of DNA Medicine Institute, a medical innovation laboratory. He has been honored as Esquire magazine’s Best and Brightest, one of MIT Technology Review’s Top 100 Innovators, and an XPRIZE winner. His work has contributed to the birth of next-generation sequencing, health monitoring in remote environments, and therapeutics. Dr. Chan holds over 60 patents and publications, with work funded by the NIH, NASA, and USAF. Dr. Chan received an A.B. in Biochemical Sciences from Harvard College summa cum laude in 1996, received an M.D. from Harvard Medical School with honors in 2007, and trained in medicine at the Brigham and Women’s Hospital. He is one of few individuals who has been in zero gravity.