
BY ANISH KOKA
The NIH recently announced $1.2 billion dollars in funding for research on Long COVID. This is in part because of a faction of scientists that have mined electronic health record databases to find evidence that the long term impacts of COVID on a variety of different organ systems is significant.
I have some concerns when it comes to the cardiac complications discussed related to Long COVID.
One of Dr. Al-Aly’s long COVID papers illustrates the issues with using large datasets to differentiate signal from noise. The authors used the US Department of Veterans Affairs national healthcare databases to build a cohort of 153,760 US veterans who survived the first 30 d of COVID-19 and two control groups: a contemporary cohort consisting of 5,637,647 users of the US Veterans Health Administration (VHA) system with no evidence of SARS-CoV-2 infection and a historical cohort (pre-dating the COVID-19 pandemic) consisting of 5,859,411 non-COVID-19-infected VHA users during 2017. These cohorts were followed longitudinally to estimate the risks and 12-month burdens of pre-specified incident cardiovascular outcomes in the overall cohort and according to care setting of the acute infection (non-hospitalized, hospitalized and admitted to intensive care).
The question being asked here is: Does sars-cov2 result in downstream cardiovascular complications? The authors attempted to assess cardiovascular disease in those with Sars-COV2, but to know if these rates are higher than ‘normal’ a control group is needed.
In this case the control group are a contemporary cohort that were test -ve, and a historical control.
Here’s the key figure from the finding that’s been shared more than a few times:
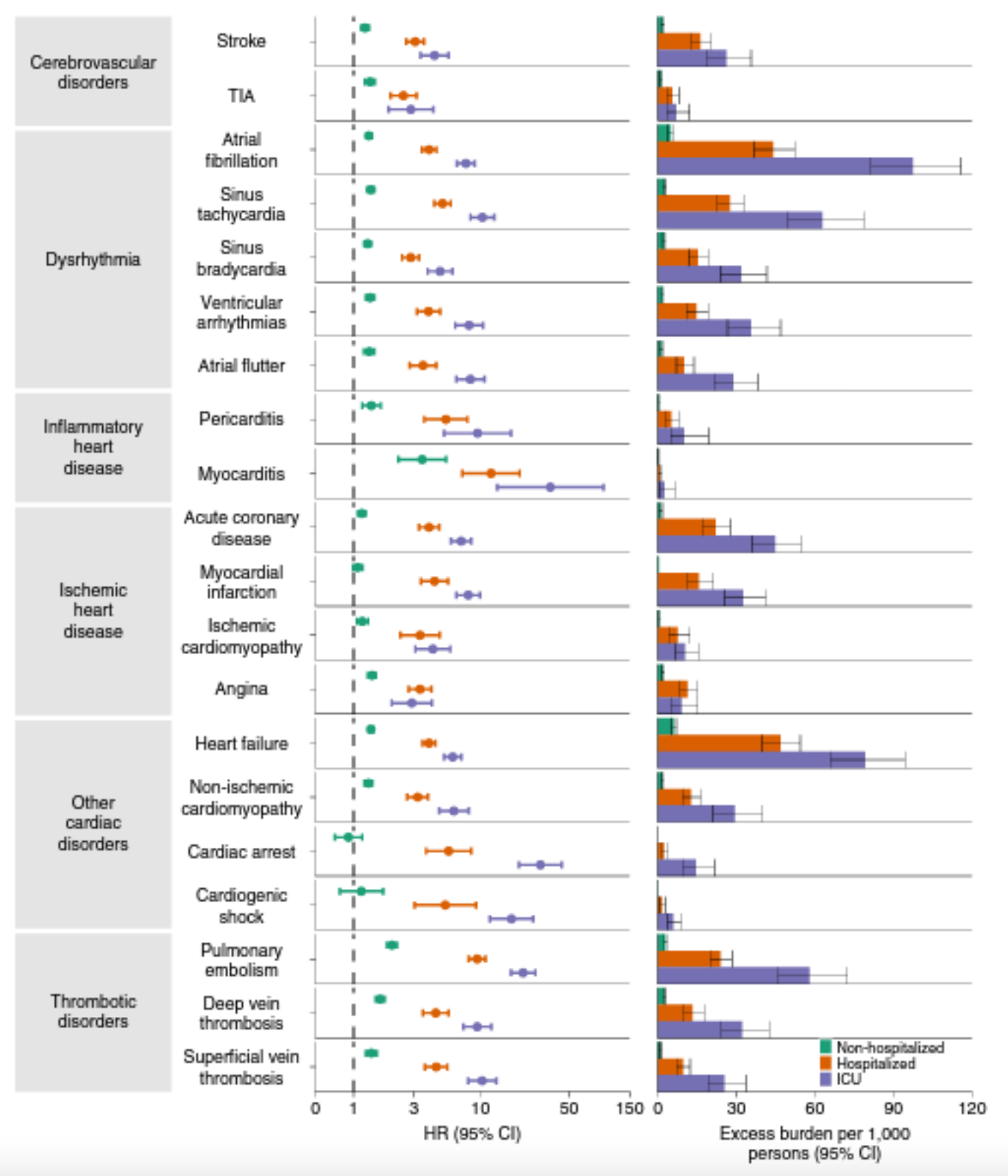
This startling figure shows that compared to a contemporary control group that did not test positive for COVID, non-hospitalized, hospitalized, and ICU cases of COVID had higher rates of a number of vascular and cardiovascular conditions.
You have to be really quite careful about creating a good control group here. To be a negative control, you simply need to never have had a positive covid test reported in the electronic health record being analyzed by Dr. Al-Aly. If you had COVID and were never tested, you would be in the negative control group. If you had COVID and tested positive outside of the electronic health record the researchers had access to, you were also in the negative control group. So it is 100% probable that the without COVID group includes a number of people who actually had COVID. This applies much more to the group with mild covid, as these are the people most likely not to have come to the attention of the medical system.
The other bias that the authors think they corrected for, but I still think is problematic relates to the fact that people that are diagnosed with COVID get a lot more diagnostic tests. Once you’re brought to the attention of the health system, you suddenly have a lot more diagnoses added to your record!
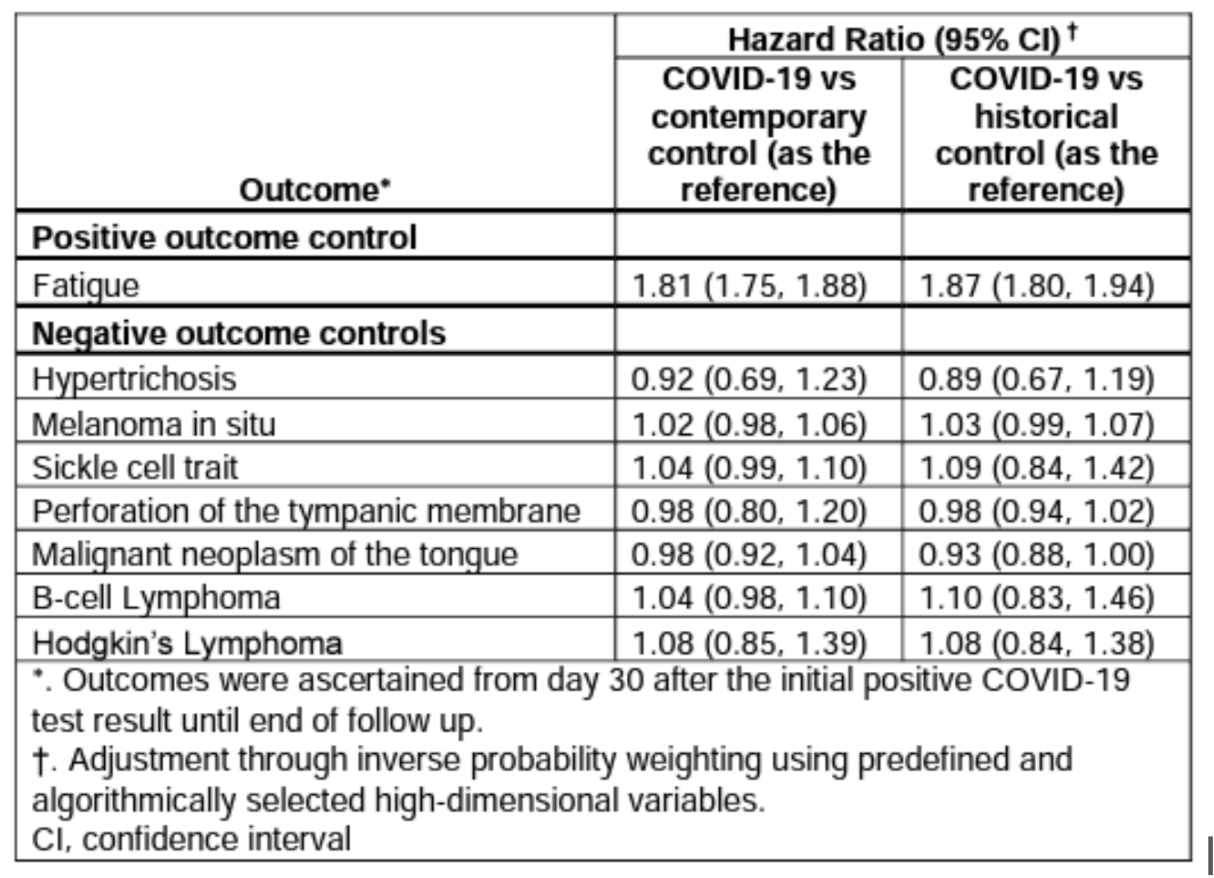
The authors of this nature study would point to their use of negative controls to limit this particular confounder. Basically the authors evaluated other diagnoses that aren’t related to see if these diagnoses occurred more. The diagnoses studied are below, but unfortunately the -ve controls picked aren’t ones we would expect to be coded more based on the imaging that happens after a covid diagnosis is made. If you test +ve for covid, you are more likely to have your vitals checked. On these vitals you are more likely to have an elevated heart rate. This is something known as sinus tachycardia. You are not more likely to have your eardrums checked to see if they’re perforated , however. The better negative control would be a diagnosis that would increase in prevalence with more cardiac imaging in sick ICU patients, but doesn’t happen more as a result of COVID. One such diagnosis would be new valvular calcific stenosis. Calcific stenosis of valves takes years to form, and wouldn’t happen acutely because of covid. Since most covid patients who get admitted to the ICU will get cardiac imaging..a rise in diagnoses of valve disease would indeed suggest more diagnoses of heart attacks, or heart failure are a result of simply more imaging, as opposed to COVID causing more heart attacks. There are major problems here with negative controls that make the made-for-TV conclusions of this study incredibly fragile.
To conclude from this expedition that there will be more long term cardiovascular complications from contracting COVID requires believing that a disease that did not cause a tsunami of patients to arrive at cardiology clinics during the pandemic will now result in long term cardiac and vascular damage. (While a separate faction of motivated cardiac imaging researchers do seem to believe they’ve uncovered definitive proof of significant cardiac damage from COVID they would be quite wrong.)
While the NIH’s $1 billion dollar initiative will clearly be causally linked with Champagne bottles being opened in the offices of long COVID researchers, the taxpayers funding this enterprise should demand a lot more answers than researchers like Dr. Al-Aly can provide.
Anish Koka is a Cardiologist. Follow him on Twitter @anish_koka.