That is the title of a recent paper by Hernandez and Hung (2024). The article provides an excellent review of how drugs get reimbursed in the US and who the key players are. I provide an abbreviated summary below, but do read the full article.
The players
- Manufacturers research, develop, and bring new drug products to market.
- Wholesalers act as distributors of drug products. Wholesalers purchase the drug product from manufacturers and distribute it to pharmacies and health care providers.
- Pharmacies dispense self-administered prescription drugs to patients. Types of pharmacies include retail, mail order, online, specialty, and institutional.
- Health care providers prescribe all prescription drugs and administer drug products that need to be provided under the supervision of a health care professional (e.g., infusions, some injections).
- Patients are consumers of drug products from health care providers (physician-administered) or pharmacies (self-administered).
- Health plans or insurers (aka payers) provide coverage for medical and pharmacy services to their members. Private insurance is funded by employers and employees; public insurance (eg, Medicare, Medicaid) are funded with tax dollars. Drugs dispensed to patients at outpatient pharmacies are covered under the pharmacy benefit of an insurance policy, whereas provider-administered drugs are covered under the medical benefit. Health plans or insurers often subcontract the administration of pharmacy benefits to pharmacy benefit managers (PBMs). Health plans or insurers are also referred to as payers.
- PBMs administer the pharmacy benefit of insurance policies and design formularies, negotiate discounts with manufacturers, establish pharmacy networks, negotiate contracts with pharmacies or pharmacy services administrative organizations, and process and pay claims.
- Group purchasing organizations (GPO) are buying consortiums that aggregate purchasing power among their members, allowing them to negotiate better discounts than they would access on their own. GPOs include health systems, clinics, specialty pharmacies, retail pharmacies, and PBMs.
- Pharmacy services administrative organizations manage and negotiate contracts with PBMs on behalf of independent pharmacies. Some pharmacy services administrative organizations are affiliated or owned by wholesalers.
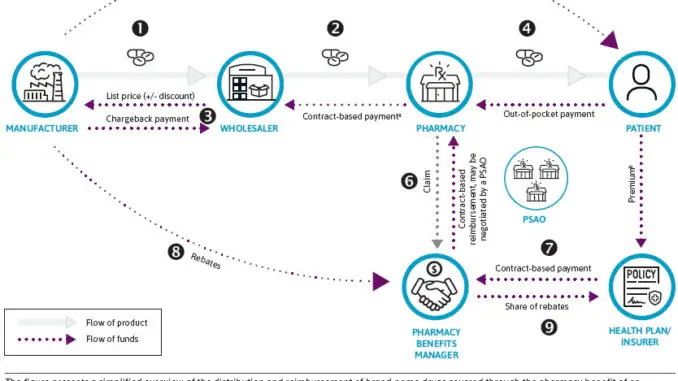
Flow of funds for drug covered by the Pharmacy Benefit
Payments between these players are summarized by the graphic below for drugs patients receive through a pharmacy. The pharmacy could be a standard free standing pharmacy (e.g., CVS, Walgreens), a pharmacy within a hospital, or even a mail-order pharmacy.
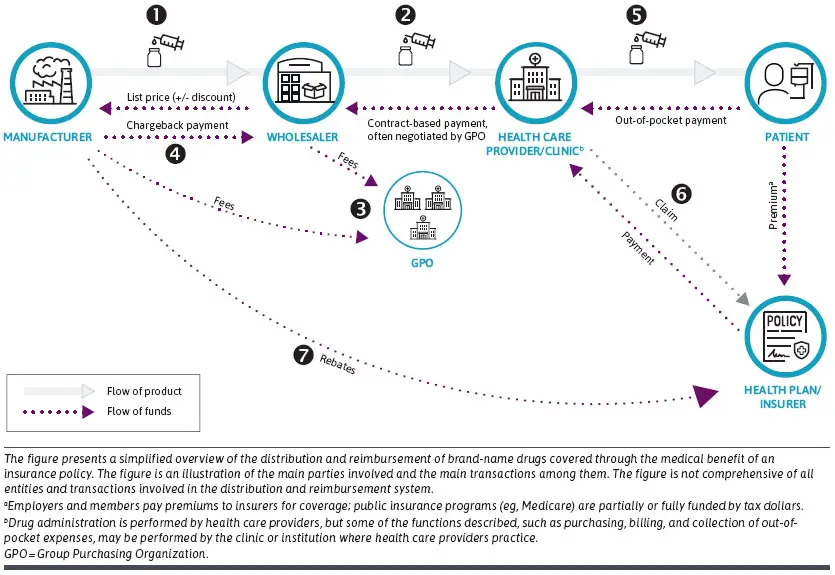
Flow of funds for drug covered by the Medical Benefit
Here, rather than pharmacies delivering drugs to patients, medical providers supply the drugs. These providers receive reimbursement both for the cost of the drug administered and also the professional services rendered to administer this drug.
Looking forward
The article also identifies a number of key themes:
- Drug prices have been rising in recent years, but rebates have been rising even more
- Federal government drug price negotiation is beginning with the Inflation Reduction Act (IRA)
- Increased vertical integration with insurers purchasing PBMs and the creation of GPOs owned by PBMs
- Health plans are increasingly moving specialty provider-administered drugs to the pharmacy benefit, through “white bagging” (having a specialty pharmacy dispense the drug and ship it to the provider) or “brown bagging” (having a specialty pharmacy dispense the drug to patients to bring to the provider for administration)
