Annals of Pharmacotherapy, Ahead of Print.
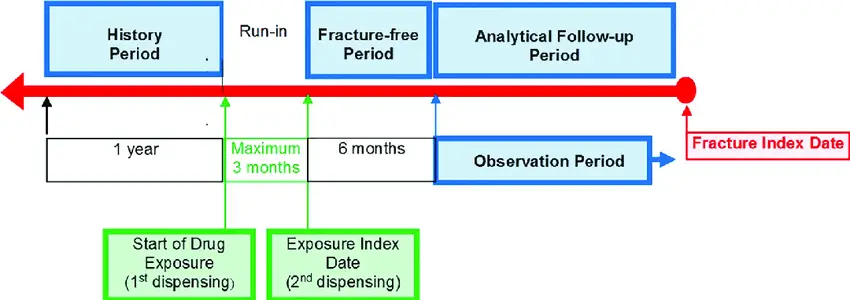
Background: Osteoporosis, which is a major public health concern, has been known to reduce health-related quality of life. Some studies have suggested that antipsychotics could perhaps cause osteoporosis by increasing serum prolactin levels. However, the association between antipsychotics and the risk for developing osteoporosis has been controversial. Objective: The present study aimed to assess the association between antipsychotic use and onset of osteoporosis in real-world settings. Methods: A multimethod data-mining approach using different algorithms and databases was used. First, disproportionality analysis was conducted using the US Food and Drug Administration Adverse Event Reporting System (FAERS) database (2004-2017) with reporting odds ratio (ROR) and information component (IC) being used to indicate a signal. Furthermore, a sequence symmetry analysis using data from a large Japanese administrative claims database (2005-2017; JMDC Inc, Japan) was conducted. Short-term intervals (ie, 12, 24, and 36 months) were set to investigate the association between antipsychotic use and onset of osteoporosis using the adjusted sequence ratio (SR) to indicate a signal. Results: No potential association between osteoporosis and all antipsychotics was observed in the FAERS database, except for perphenazine, which exhibited significant signals using both ROR and IC. Moreover, no potential association between osteoporosis and antipsychotics was observed in the JMDC claims database, except for sulpiride and aripiprazole. None of the antipsychotics indicated significant signals using all analyzed items (ROR, IC, and adjusted SR). Conclusion and Relevance: Real-world data show no association between antipsychotic use and the onset of osteoporosis. Further pharmacoepidemiological studies are needed for causality assessment.
Background: Osteoporosis, which is a major public health concern, has been known to reduce health-related quality of life. Some studies have suggested that antipsychotics could perhaps cause osteoporosis by increasing serum prolactin levels. However, the association between antipsychotics and the risk for developing osteoporosis has been controversial. Objective: The present study aimed to assess the association between antipsychotic use and onset of osteoporosis in real-world settings. Methods: A multimethod data-mining approach using different algorithms and databases was used. First, disproportionality analysis was conducted using the US Food and Drug Administration Adverse Event Reporting System (FAERS) database (2004-2017) with reporting odds ratio (ROR) and information component (IC) being used to indicate a signal. Furthermore, a sequence symmetry analysis using data from a large Japanese administrative claims database (2005-2017; JMDC Inc, Japan) was conducted. Short-term intervals (ie, 12, 24, and 36 months) were set to investigate the association between antipsychotic use and onset of osteoporosis using the adjusted sequence ratio (SR) to indicate a signal. Results: No potential association between osteoporosis and all antipsychotics was observed in the FAERS database, except for perphenazine, which exhibited significant signals using both ROR and IC. Moreover, no potential association between osteoporosis and antipsychotics was observed in the JMDC claims database, except for sulpiride and aripiprazole. None of the antipsychotics indicated significant signals using all analyzed items (ROR, IC, and adjusted SR). Conclusion and Relevance: Real-world data show no association between antipsychotic use and the onset of osteoporosis. Further pharmacoepidemiological studies are needed for causality assessment.
