
Nationally, deaths increased by 27 percent from the previous week. More than a third of long-term-care-facility deaths were reported in the Midwest; Michigan, Illinois, and Minnesota each reported more than 200 deaths. In the South, Texas reported the highest number of new deaths, 360.

COVID-19 data reporting is still catching up from expected lags that occurred around Thanksgiving, as many state health departments shifted their reporting schedules or closed because of the holiday. These delays might make this week’s newly reported cases and deaths seem unusually high compared with the previous week. We expect the data-reporting process from states to smooth out this week before another period of irregularity around Christmas.
[Read: The Final Pandemic Surge Is Crashing Over America]
The Northeast is beginning to see COVID-19 case increases reminiscent of that region’s devastating outbreaks at the beginning of the pandemic. The 838 deaths the region reported in the week between November 26 and December 3 is the largest increase since early June, and 38 percent of these deaths came from Pennsylvania. That state last week hit a six-month high in the number of recorded cases, with 4,970. That represented more long-term-care-facility cases than any state in the nation except California, which reported 5,075. Pennsylvania’s new cases doubled the previous week’s increase, but it’s possible that a post-Thanksgiving backlog is artificially inflating these numbers.

The COVID Tracking Project hasn’t been able to obtain current data about the number of people living in Pennsylvania’s long-term-care facilities. But if numbers have remained relatively constant over the past five years, we can estimate, based on a 2015 number of residents in LTC facilities, that nearly 30 percent of people living in these environments have gotten COVID-19. Pennsylvania combines staff and residents in its long-term-care-facility death counts, but based on an analysis of our data set, we know that 99 percent of all COVID-19 deaths from LTC facilities are among residents. We estimate that nearly one in five Pennsylvania long-term-care residents who contracted COVID-19 has died. We’re also keeping an eye on Colorado, which recorded a six-month high for both cases and deaths.

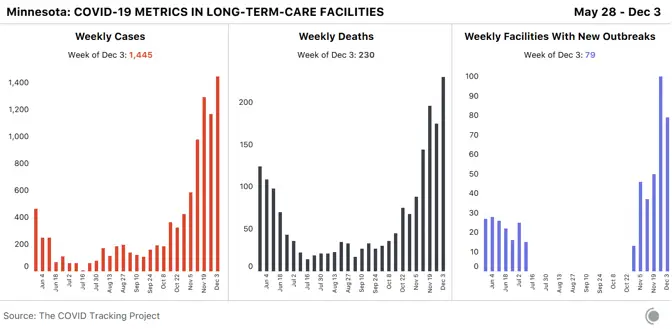
Last week, Minnesota reported its highest number of long-term-care-facility cases and deaths to date. Unlike many other states, Minnesota’s information is not traceable at the facility level. At the beginning of the summer, when Minnesota was reporting that about 80 percent of its COVID-19 deaths were from long-term-care facilities, officials refused to report cases and deaths at specific nursing homes and other long-term-care facilities, citing privacy concerns. Though Minnesota does provide a list of facility names with current COVID-19 outbreaks, more granular data—such as how many cases and deaths are occurring within each facility—are still not available.
Long-term-care facilities report COVID-19 data through the CDC’s National Healthcare Safety Network (NHSN), and this week, NHSN announced changes to COVID-19 data definitions. These changes include the removal of “suspected” cases, and a shift from “confirmed cases” to “positive cases.” NHSN also said that positive cases can be determined by a positive antigen-test result or by the gold-standard PCR test. The changes are noteworthy because in July, the Trump administration started sending rapid antigen tests to nursing homes to regularly test residents and staff.
One problem: Antigen tests can identify a probable case, not a “confirmed case,” according to guidance provided by the Council of State and Territorial Epidemiologists. When cases classified as “suspected” are removed, it will be harder for the public to understand exactly what types of tests are being used in long-term-care facilities and how residents and staff are faring.
On December 3, a collection of long-term-care-advocacy organizations sent a letter to the Biden-Harris Transition COVID-19 Advisory Board asking the incoming administration to include individuals with expertise in aging and disability on COVID-19-related boards or task forces; the letter also asked the incoming administration to form a task force centered on COVID-19’s impact on long-term-care facilities.
Tomorrow, the U.S. Food and Drug Administration will hold a meeting of its Vaccines and Related Biological Products Advisory Committee to discuss Pfizer/BioNtech’s request for emergency-use authorization for its vaccine. Shortly after, the CDC’s Advisory Committee on Immunization Practices will hold emergency meetings on December 11 and 13 to provide official recommendations for use of the Pfizer/BioNtech vaccine among the highest-priority groups—health-care workers and long-term-care-facility residents and staff.
Artis Curiskis, Jessica Malaty Rivera, Sarah McLaughlin, Kara Oehler, Aarushi Sahejpal, Sara Simon, and Peter Walker contributed to this report.
