It is common knowledge that COVID risk goes up with age, but how steeply it rises is still astounding to see after two years of living and dying with this coronavirus. Compared with someone in their 20s, a person over 65 years old is not slightly more likely to die of COVID but at least 65 times more likely to die of COVID. Over age 75, they become 140 times more likely to die. Over age 85, they are 340 times more likely to die.
No other basic fact of life matters as dramatically as age for COVID. Other common factors associated with risk—race, diabetes, cancer, immunosuppression—make the disease deadlier by a factor of “only” two to four. These are significant differences that influence how doctors care for COVID. But age increases risk by entire orders of magnitude. It is simply in a league of its own.
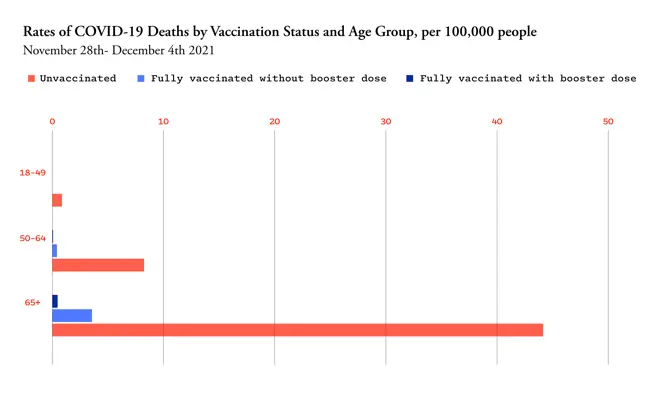
This is why, even though America’s vaccination and booster rates look better in the older groups compared with the young, they are still too low. As a result, deaths in the United States are still too high. The unvaccinated elderly have been dying at incredibly high rates, but even the vaccinated and unboosted elderly are still dying of COVID at four times the rate of unvaccinated adults under 49. A booster cuts that risk dramatically. This is based on detailed CDC data in early December, which are the latest available. Age continues to be the driver of COVID’s brutal math with Omicron, though: In 2022 so far, three-quarters of COVID deaths in America have been in people 65 and older, 93 percent in people 50 and older.
“Our vaccination rates, as well as booster use, in people aged 60- or 65-plus are woefully low and exposes a tremendous amount of vulnerability to severe disease, hospitalizations, and deaths,” says Eric Topol, the director of the Scripps Research Translational Institute. “This has been one of the most serious disappointments in our performance.”
Persuading vaccine holdouts among the elderly at this point is hard, but COVID risk is so high for this group that it’s very much worth trying. Boosting the already vaccinated, by contrast, should be eminently doable, as the group is clearly open to vaccines. With America’s vaccination campaign sputtering, this is where efforts are likely to have the biggest payoff. Hospitalizations and deaths are so heavily concentrated in older people, in fact, that a single course of a vaccine in someone over 65 might have the same effect on those numbers as dozens given to the young. The U.S. fortunately has enough vaccine doses that we don’t have to choose whom to vaccinate. But as immunity in the unboosted continues to wane and persuading new people to get immunized becomes harder, a focused effort on vaccinating and boosting the elderly can have an outsize impact on preventing hospitalizations and deaths in the next COVID wave. The most severe COVID outcomes are not the only ones worth preventing, but they are the most urgent if we don’t want hospitals and morgues filling up again.
Consider the current Omicron wave, which has been far deadlier in the U.S. than in other highly vaccinated and boosted countries. The U.S. has reached 80 percent of its pre-vaccine peak in daily deaths, compared with only 20 to 30 percent of peaks reached in other countries. America has not only a lower overall vaccination rate but lower coverage in the elderly. England, for example, has achieved 96 percent full-vaccination coverage in people over 65. In the U.S., this number is 88.5 percent, with big geographic variations that range from 79 percent in Arkansas to 95 percent in Vermont.
These percentages may all look high, but they represent very different levels of remaining risk. “People see 90 and 95 percent as not very much” of a difference, says Adam Kucharski, an infectious-disease modeler at the London School of Hygiene and Tropical Medicine. He prefers to invert the number. “Think of it as: There’s 5 percent unprotected or 10 percent unprotected.” That doubles the pool of people over 65 who are at high risk for hospitalization and death. In a massive epidemic wave like that of Omicron, hospitalizations and deaths can scale up very quickly.
Moreover, the U.S. does lag quite far behind other wealthy countries in boosters for people over age 65. England has boosted 92 percent of its elderly population, while the U.S. is at 65 percent. Even highly vaccinated Vermont is at only 78 percent of seniors boosted. Boosters are necessary because waning immunity and new variants have eroded the spectacular effectiveness seen in 2020’s vaccine trials: Six months-plus after vaccination, two mRNA doses mitigate hospitalizations due to Omicron by only 57 percent across all ages. A booster gets that back up to 90 percent. This extra protection is especially crucial for the elderly because their immune systems tend to mount less robust initial responses to the vaccines. The effects of a third dose may eventually wane too; if any group will need regular boosters in the future, it is again older people—and not just the most elderly.
How old is old when it comes to COVID risk? I’ve so far focused on age 65 because the CDC uses this threshold for a lot of vaccination data and because it represents the highest-risk group. But other countries have been more ambitious. Denmark, which dropped coronavirus restrictions amidst sky-high Omicron cases, has been able to do so because it has excellent booster coverage down to age 50. Ninety-five percent of this group has been fully vaccinated, and over 90 percent have had three doses. As a result, Omicron has “been not so bad in terms of health impact,” says Lone Simonsen, an epidemiologist at Roskilde University in Denmark. Cases have fallen a bit off their peak in Denmark, but excess mortality is already back to near zero. To minimize hospitalizations in addition to deaths, Simonsen says the percent vaccinated over age 40 is crucial too, because the median age of COVID hospitalization is lower than that of death. (Hospitalization risk also rises steeply with age, just not quite as steeply as death risk.) Among Danes in their 40s, vaccine coverage is not universal but still very good: 90 percent are fully vaccinated, and three-quarters are boosted. Vaccination uptake among Americans 40 to 65 is even further behind, with even the fully vaccinated rate lingering in the 70s.
How could the U.S. maximize vaccine and booster uptake in older Americans? I put this question to several health-policy experts with the more modest threshold of age 65. This seemed more achievable, given the even lower uptake among middle-aged Americans, but also because nearly everyone over 65 is already on government health care—Medicare. England and Denmark have achieved such high vaccination rates in no small part because they have centralized national health-care systems. Health care in America is incredibly fragmented, but Medicare at least reaches most people over 65. In December, in fact, the Biden administration announced that it would mail all 63 million people on Medicare a letter encouraging COVID boosters—“the first time in more than 4 years” that Medicare had sent such a universal notice, the White House touted. At the same time, the agency that oversees Medicare, the Centers for Medicare & Medicaid Services (CMS), laid out a suite of other outreach efforts promoting COVID boosters.
CMS could add more direct incentives, experts say. Most Americans on Medicare are on traditional Medicare, which is a fee-for-service program that pays the bills but does not closely manage a patient’s care. CMS does have levers to influence health-care providers, though. It could, for instance, incentivize them by making the COVID vaccination and booster rates among patients a “quality measure” that helps determine how much providers are reimbursed. Medicare already does this with pneumococcal vaccines for pneumonia, says Mark McClellan, a former CMS administrator who is now a health-policy professor at Duke University.
Slightly less than half of Medicare recipients are on Medicare Advantage plans, which are run through private insurers such as Kaiser Permanente and Humana that more closely manage a patient’s care. Here, too, CMS could make COVID vaccination part of the plan’s quality measures. And these private insurers, in turn, are “closer to the patient,” says Robert Field, a health-care policy expert at Drexel University, which means they have better data to target patients who still need vaccines. “They can be using their claims data to follow up with people and say, you know, ‘We noticed you got only one shot’ or ‘You’ve gotten two shots and you need a booster,’” he told me.
Nursing homes are another potential focus of COVID vaccination. Residents are at particularly high risk for COVID, not just because of age and underlying health conditions but because they live in close quarters. Yet vaccination rates in nursing homes are not any better than in the overall elderly population: 87 percent of residents are fully vaccinated, and only 69 percent are boosted. In general, vaccination rates tend to be lower in for-profit and chain facilities, in those with high staff turnover, and in communities with low vaccination rates, according to a study published last fall. Understaffing and “organizational dysfunction” probably explain why boosters have not been prioritized, says Michael Barnett, one of the study’s authors and a health-policy professor at Harvard. Nursing homes on average turn over more than 100 percent of their staff every year. When staying fully staffed is such a big challenge, simply keeping residents “fed and giving them their meds and helping them use the bathroom—just basic daily stuff is already an overwhelming task,” Barnett told me. “Giving vaccines is a one-time intervention that doesn’t necessarily take that many person hours to figure out. But somebody has to coordinate it and organize it.”
Medicare rates the quality of nursing homes too, and CMS could also add COVID boosters to its criteria, as it has with flu and pneumococcal shots. Barnett thinks that this might not be a big enough incentive, given the long list of rating criteria already. Money, however, could be a stronger enticement, and states could also play a role. “There’s nothing stopping a state from offering direct financial incentives,” said Barnett, whether a payment per booster or a cash bonus for hitting a threshold. “To me, it’s a total no-brainer.”
These changes are individually incremental, and some may take longer to implement than we would like. But with so many hospitalizations and deaths in Americans over 65, even incremental progress is worthwhile. If immunity in this population wanes and older people need regular boosters, building this system now will make it easier to deliver shots in the future. Vaccines cannot eliminate the risk of COVID among seniors entirely, as everything gets riskier with age, be it a cold or a fall. COVID pills can help bring down hospitalizations and deaths when supply is better available, but this depends on timely testing and access. Vaccines remain our most powerful preventive tool. To avert the worst outcomes of overwhelmed hospitals and high death rates in future COVID waves, we need to get more doses to the people who need them the most. That was and still is the oldest.
