There has been much research showing that fee-for-service (FFS) leads to increased provision of medical services and capitation leads to decreased provision of medical services. My own research shows that there are system-wide effects and that the impact of capitation for primary care physicians on services may depend on whether specialists are also reimbursed via fee-for-service. However, it is not clear how increasing the proportion of reimbursement that is capitated impacts health care service provision. This is an important for a number of reasons. First, CMS is increasingly moving to alternative payment models that are looking more and more like capitation. Second, a large share of health care provision in the US is under mixed reimbursement schemes. Third, reimbursement type varies across countries; or instance, in in Norway and Denmark, FFS accounts for 70%–80% of the total reimbursement but in the family health organization scheme in Ontario, Canada, FFS part covers only 10% of reimbursement.
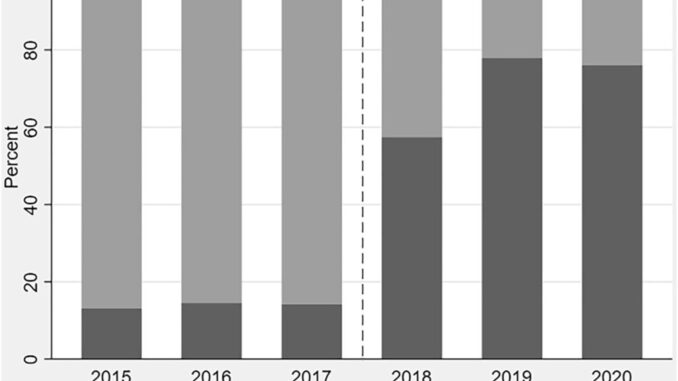
To examine this question, a paper by Skovsgaard et al. (2023) uses a change to general practitioner reimbursement in Denmark 2018, specifically for treating patients with Type 2 diabetes. The specific changes were as follows:
The new lump-sum capitation for patients with type 2 diabetes was set at DKK 2045 (approx. US$ 280) per patient per year in addition to the basic lump-sum capitation per patient. This amount was higher than the corresponding average FFS which were discontinued for patients with type 2 diabetes. Notice that the capitation replaced FFS for all contacts for patients with type 2 diabetes, not only contacts related to diabetes. The remaining FFS fees outside the reform comprise a range of supplementary services including guideline-recommended monitoring of HbA1c, influenza vaccination and tests for microalbuminuria by assessing protein in urine. These guideline-recommended services are process quality measures which indicate if changes in service provision affects quality of care
https://onlinelibrary.wiley.com/doi/full/10.1002/hec.4736
In terms of empirical strategy, the authors perform a difference in-difference approach. The pre-post is differences between the outcomes and interest before and after an annual control visit. The change in services is examined for annual control visits in 2018-2019 as compared to 2015-2016. The outcomes or interest were: (i) number of visits (in-person, phone and email), (ii) number of diabetes-related lab tests (e.g., urine sticks, and HbA1c tests), (iii) flu vaccinations, (iv) supplemental services related to diabetes, and (v) supplemental services not related to diabetes.
Using this approach, authors find that:
The effect of enrolling a patient in the new scheme is negative with a reduction of around 2% as compared to the baseline value (ATT = −0.27%; −1.9%)…the effect of enrollment on supplementary services (s) related to diabetes guidelines is negative at a magnitude of around 4% reduction as compared to baseline (ATT = −12.29%; −4.4%)…The results [also] indicate reductions 5.0%, 5.4%, and 4.2% as compared to baseline for urine sticks, blood sample, and influence vaccination, respectively.
To verify the robustness of their findings, the authors looked at services not included in the new reimbursement scheme (e.g., lipid lowering medications) and found no effect for this placebo test.
The authors hypothesize that the reason the reductions in supplemental services were larger in magnitude than the reduction in visits was because of a substitution away from face-to-face visits toward phone and email contacts that do now allow for immediate provision of supplemental services.
You can read the full paper here.