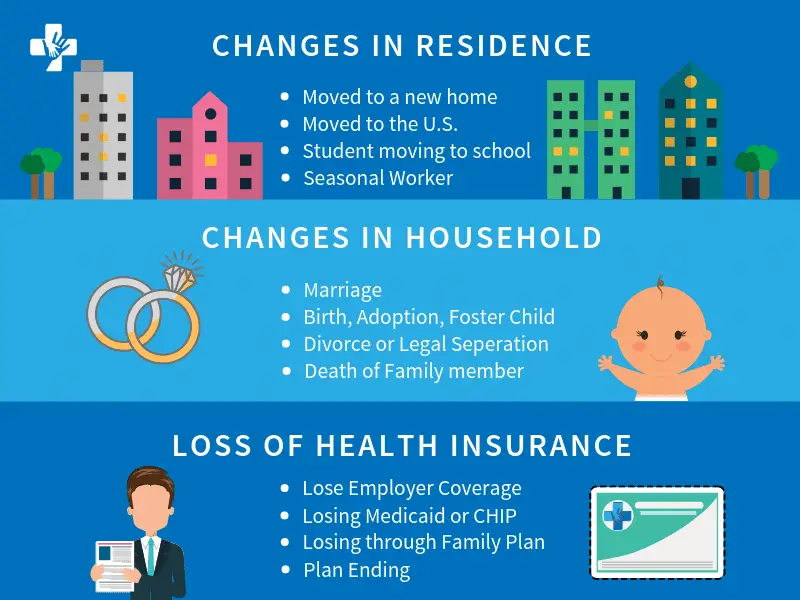
You may qualify for a Special Enrollment Period to enroll in or change health plans if you or anyone in your household lost qualifying health coverage in the past 60 days or expects to lose it in the next 60 days.
Coverage losses that may qualify
- Losing job-based coverage, like through your employer or the employer of a family member.
- Losing individual health coverage for a plan or policy you bought yourself, like if your plan is discontinued or you lose eligibility for a student health plan.
- Losing Medicaid or Children’s Health Insurance Program (CHIP) coverage, like if a change in household income makes you ineligible for Medicaid or your child ages off CHIP.
- Losing Medicare eligibility, like if you’re no longer eligible for premium-free Medicare Part A.
- Losing coverage through a family member, like if you turn 26 and can no longer be on a parent’s plan.
Not sure your coverage loss counts? Answer a few questions to see if you qualify.
Ready to apply through a Special Enrollment Period?
- Create an account or log into an existing one.
- Before you apply, you can preview 2020 plans and prices based on your income.
Note: If you’re not eligible to apply with a Special Enrollment Period for the rest of 2020, you can apply for a 2021 health plan Sunday, November 1 through Tuesday, December 15, 2020.
