Cotiviti’s Signature Series features interviews with senior health plan leaders on how to improve clinical and financial outcomes in healthcare.
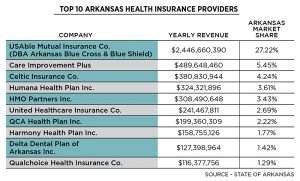
To address rising healthcare costs and nurture care that drives positive patient outcomes, healthcare stakeholders are looking for ways to reward providers for value, not volume of services. But getting to this point is not a straightforward path as Arkansas Blue Cross and Blue Shield, the largest payer in its state, found out firsthand.
In a recent webinar, Arkansas Blue Cross executive vice president and chief health management officer Steve Spaulding explained how his organization approaches value-based payment, leveraging Cotiviti’s Network Intelligence solution to define and compare high-value care through standardized provider benchmarks.

