Standard
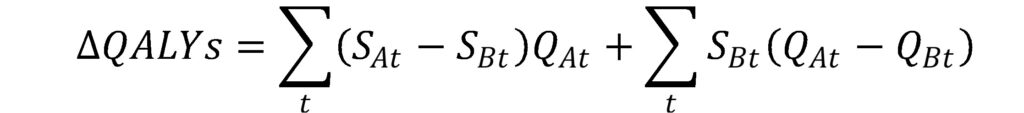
quality approach compares the difference in QALYs which is a function of survival
and quality of life during each survival period. Consider the comparison of treatments A and
B, where treatment A is the novel treatment and treatment B is the standard of
care. Under the QALY based approach this is calculated as

Where the
S term is the survival probability in a given year and the Q term is the
quality of life in that year. One can add and subtract a term to decompose this
equation into:


Under an
equal value of life years gained as developed by Nord
et al., 1999 the authors assume that the quality of life improvement for
any life year’s gained is 1, (i.e., Q_At=1 in the first part of the
equation).
A new approach–Health Years in Total (HYT)–was proposed by Basu et al. (2021). HYT can be estimated starting with a similar decomposition, but Basu and co-authors assume that quality of life is equal to 1 for any survival gain in the second part of the equation.



Examples
of how to calculate these values can be found in a spreadsheet here.
Although
it appears that the authors are now double-counting quality of life gains that
occur during survival extension time period, the authors argue that this is not
the cas since they assume that quality of life and survival gains are separate in
nature and there is a linear substitution between then. The specific axiomatic foundation of HYT
requires two key assumptions:
utility independence and constant proportional
trade-off.
- Utility independence. Preferences over lotteries on longevity do not depend on fixed
health levels and conversely that preference over lotteries on health levels do
not depend on fixed longevity. - Constant proportional trade-off. Implies that the fraction of a person’s
remaining life that the person would trade-off for a given improvement in health does not depend on
the number of years of life that remain
Looking
at these
examples, HYT has the advantage over QALYs in that survival gains that accrue
to very sick individuals are not downweighted due to these individuals having
lower quality of life. In fact, HYT operates
very similar as the equal value of life years gained (evLYG) approach. The main difference between HYT and evLYG occurs
when there quality of life improvements occur differentially in the period over
which the standard of care occurs and the survival period over weight the new
treatment improves survival. Note that HYT
does place less value on treatments that generate only quality of life gains,
but no survival gains. In these cases,
HYTs gained would be equivalent to QALYs gained but the value of an HYT gained (which
ranges between 0 and 2) is less than the value of a QALY (which ranges from 0
to 1).
A key
question is what willingness to pay threshold should be used with HYT. The authors use the Tufts cost effectiveness
analysis registry and find that commonly used thresholds of $50,000, $100,000
and $150,000 per QALY correspond to the 53rd, 71st and 78th
percentiles in terms of the log cost per incremental QALY distribution. The corresponding figures for the log cost
per incremental HYT are $34,000, $74,000 and $89,000 respectively; this values
are very similar to the evLYG approach.
When considering these 3 metrics—cost per incremental QALY, cost per evLYG, cost per HYT gained—each has their pros and cons. In my opinion, however, HYT should be considered a modification of the evLYG framework that has the benefit of taking into account in some fashion quality of life benefits that accrue during the extra survival years. None of these metrics are perfect, but each of them is useful.
