That’s according to a new data brief from actuarial consulting firm Milliman, commissioned by the Better Medicare Alliance (BMA).
“This analysis provides unique insight into the ways that Medicare Advantage (MA) continues to innovate and enhance benefit offerings, even in the face of the extraordinary circumstances presented by the COVID-19 pandemic,” BMA President and CEO Allyson Y. Schwartz said in a statement.
Supplemental benefits like vision exams, dental coverage or fitness perks have been an important differentiator among MA plans since the program’s inception, the data brief notes.
Over the past few years, however, such benefits have become even more important to the MA world. In 2019, the U.S. Centers for Medicare & Medicaid Services (CMS) started allowing plans to offer benefits like non-medical home care, transportation support, adult day services and more.
With expanded flexibility from CMS, supplemental benefits have additionally become important in home care circles, with many operators looking to land business from MA payers for the very first time.
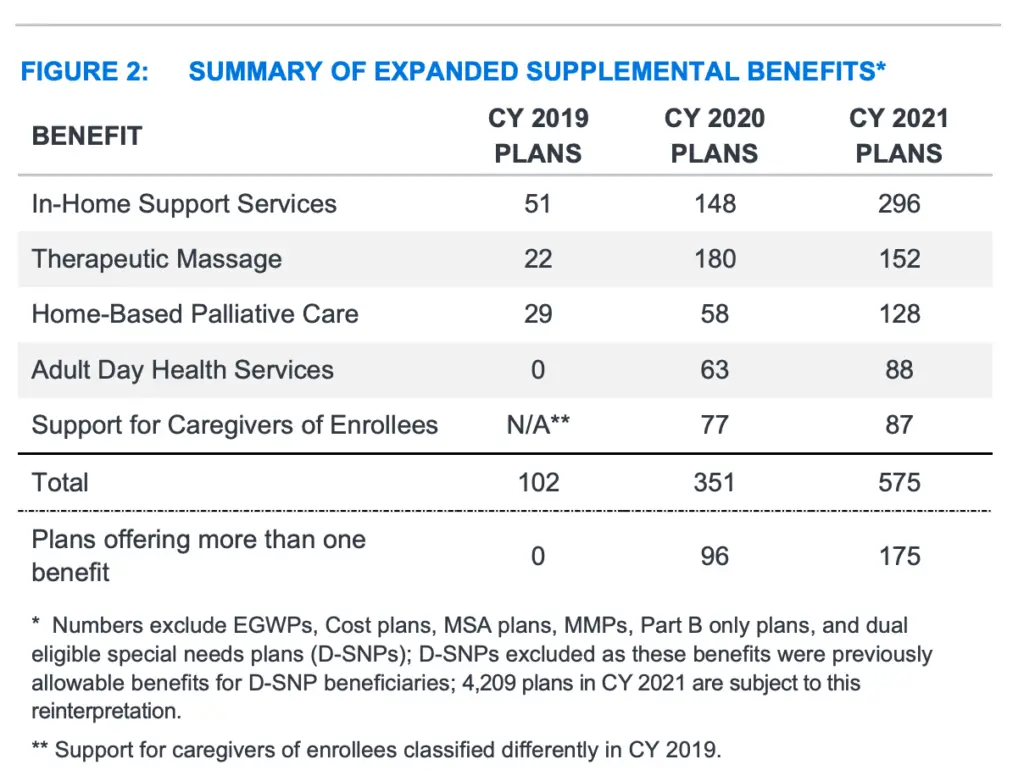
From 2019 to 2021, the number of MA plans offering in-home support services as part of their expanded supplemental benefits has climbed from 51, to 148, to 296 each year. The number of plans offering home-based palliative care has similarly jumped from 39, to 58, to 128 over that time.
In 2019, not a single MA plan offered adult day health services as an expanded supplemental benefit. This year, 88 plans are offering such services.
Benefits that are most widely offered in Medicare Advantage still include vision, hearing, fitness and dental care. But, 57% of MA plans now provide a meal benefit in 2021, while 46% of plans offer transportation to and from physician appointments.
Meal support and transportation are key services provided by many home care agencies across the U.S.
Apart from the benefits themselves, the BMA-Milliman data brief also examines the clinical conditions that MA plans most often target under the Special Supplemental Benefits for the Chronically Ill (SSBCI) pathway.
Home care operators can use the information to compare the needs of their client population with the needs of plans’ enrollees.
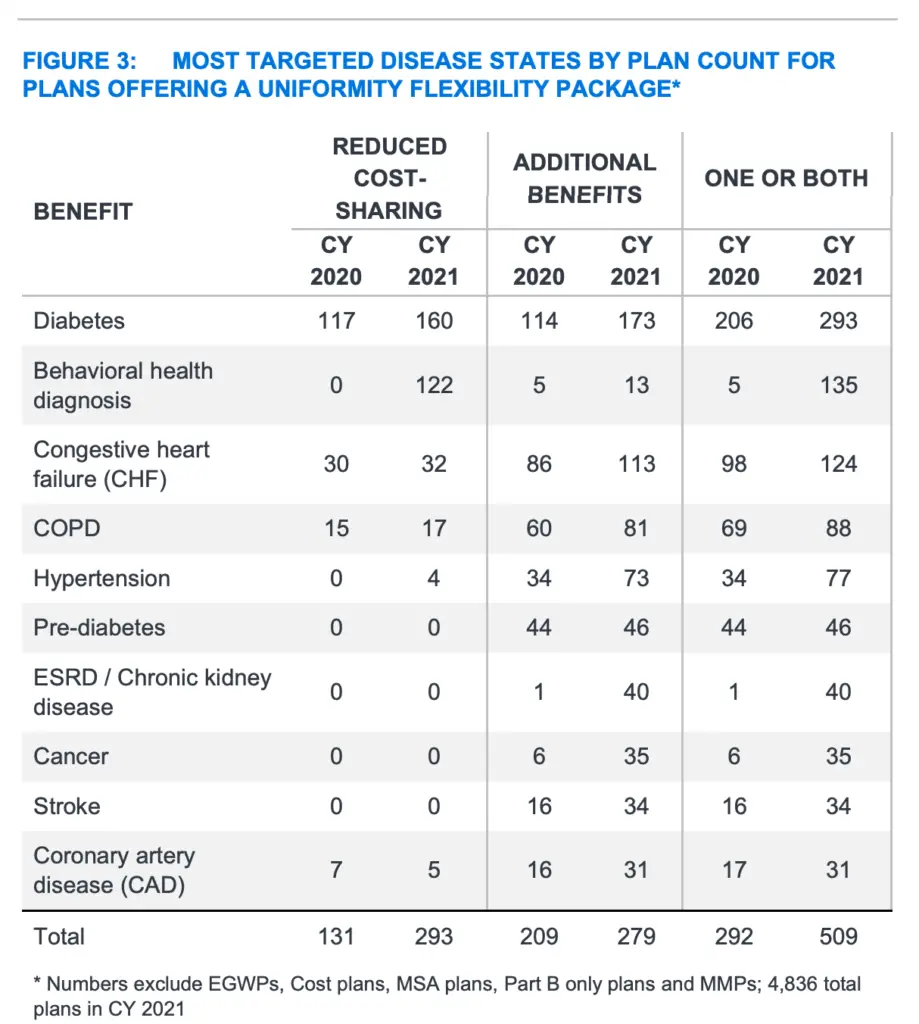
By far, beneficiaries with diabetes were the most targeted population for SSBCI. For 2021, 293 MA plans are offering reduced cost-sharing or additional benefits to support diabetic beneficiaries in managing their chronic condition. Combined, those plans cover nearly 1.5 million total enrollees.
A large number of MA plans — 135, to be exact — are also leveraging SSBCI for behavioral health diagnoses such as anxiety, depression and substance-use disorder.
Congestive heart failure and COPD are also among the most-targeted disease groups under SSBCI.
“More than 500 Medicare Advantage plans provide reduced cost-sharing, expanded benefits, or some combination of the two in order to help meet the needs of over 2.2 million beneficiaries,” Schwartz said. “Diabetics, those facing behavioral health challenges and beneficiaries with congestive heart failure and COPD are among those most helped by this important flexibility.”
The post Top Clinical Conditions Targeted by Medicare Advantage Plans Under SSBCI appeared first on Home Health Care News.